Function
Role in CO
2 transport
Recall that respiration, as illustrated schematically here with a unit of carbohydrate, produces about as many molecules of carbon dioxide, CO2, and it consumes of oxygen, O2.
Thus, the function of the circulatory system is as much about the transport of carbon dioxide as about the transport of oxygen. As stated elsewhere in this article, most of the carbon dioxide in the blood is in the form of bicarbonate ion. The bicarbonate provides a critical pH buffer. Thus, unlike hemoglobin for O2 transport, there is a physiological advantage to not having a specific CO2 transporter molecule.
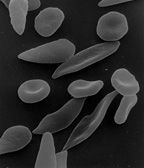
Red Blood cells, nevertheless, play a key role in the CO2 transport process, for two reasons. First, because, besides hemoglobin, they contain a large number of copies of the enzyme carbonic anhydrase on the inside of their cell membrane. Carbonic anhydrase, as its name suggests, acts as a catalyst of the exchange between carbonic acid and carbon dioxide (which is the anhydride of carbonic acid). Because it is a catalyst, it can affect many CO2 molecules, so it performs its essential role without needing as many copies as are needed for O2 transport by hemoglobin. In the presence of this catalyst carbon dioxide and carbonic acid reach an equilibrium very rapidly, while the red cells are still moving through the capillary. Thus it is the RBC that ensures that most of the CO2 is transported as bicarbonate. At physiological pH the equilibrium strongly favors carbonic acid, which is mostly dissociated into bicarbonate ion.
The H+ ions released by this rapid reaction within RBC, while still in the capillary, act to reduce the oxygen binding affinity of hemoglobin, the Bohr effect.
The second major contribution of RBC to carbon dioxide transport is that carbon dioxide directly reacts with globin protein components of hemoglobin to form carbaminohemoglobin compounds. As oxygen is released in the tissues, more CO2 binds to hemoglobin, and as oxygen binds in the lung, it displaces the hemoglobin bound CO2, this is called the Haldane effect. Despite the fact that only a small amount of the CO2 in blood is bound to hemoglobin in venous blood, a greater proportion of the change in CO2 content between venous and arterial blood comes from the change in this bound CO2. That is, there is always an abundance of bicarbonate in blood, both venous and arterial, because of its aforementioned role as a pH buffer.
In summary, carbon dioxide produced by cellular respiration diffuses very rapidly to areas of lower concentration, specifically into nearby capillaries. When it diffuses into a RBC, CO2 is rapidly converted by the carbonic anhydrase found on the inside of the RBC membrane into bicarbonate ion. The bicarbonate ions in turn leave the RBC in exchange for chloride ions from the plasma, facilitated by the band 3 anion transport protein colocated in the RBC membrane. The bicarbonate ion does not diffuse back out of the capillary, but is carried to the lung. In the lung the lower partial pressure of carbon dioxide in the alveoli causes carbon dioxide to diffuse rapidly from the capillary into the alveoli. The carbonic anhydrase in the red cells keeps the bicarbonate ion in equilibrium with carbon dioxide. So as carbon dioxide leaves the capillary, and CO2 is displaced by O2 on hemoglobin, sufficient bicarbonate ion converts rapidly to carbon dioxide to maintain the equilibrium.
Secondary functions
When red blood cells undergo shear stress in constricted vessels, they release ATP, which causes the vessel walls to relax and dilate so as to promote normal blood flow.
When their hemoglobin molecules are deoxygenated, red blood cells release S-nitrosothiols, which also act to dilate blood vessels, thus directing more blood to areas of the body depleted of oxygen.
Red blood cells can also synthesize nitric oxide enzymatically, using L-arginine as substrate, as do endothelial cells. Exposure of red blood cells to physiological levels of shear stress activates nitric oxide synthase and export of nitric oxide, which may contribute to the regulation of vascular tonus.
Red blood cells can also produce hydrogen sulfide, a signalling gas that acts to relax vessel walls. It is believed that the cardioprotective effects of garlic are due to red blood cells converting its sulfur compounds into hydrogen sulfide.
Red blood cells also play a part in the body's immune response: when lysed by pathogens such as bacteria, their hemoglobin releases free radicals, which break down the pathogen's cell wall and membrane, killing it.
Cellular processes
As a result of not containing mitochondria, red blood cells use none of the oxygen they transport; instead they produce the energy carrier ATP by the glycolysis of glucose and lactic acid fermentation on the resulting pyruvate. Furthermore, the pentose phosphate pathway plays an important role in red blood cells; see glucose-6-phosphate dehydrogenase deficiency for more information.
As red blood cells contain no nucleus, protein biosynthesis is currently assumed to be absent in these cells.
Because of the lack of nuclei and organelles, mature red blood cells do not contain DNA and cannot synthesize any RNA, and consequently cannot divide and have limited repair capabilities. The inability to carry out protein synthesis means that no virus can evolve to target mammalian red blood cells. However, infection with parvoviruses (such as human parvovirus B19) can affect erythroid precursors while they still have DNA, as recognized by the presence of giant pronormoblasts with viral particles and inclusion bodies, thus temporarily depleting the blood of reticulocytes and causing anemia.


Comments
Post a Comment